







Welcome Back
Sign in to be closer to your community!
Follow other divas, like and comment
on their posts, message them, and see
who loved your posts!
Invalid username or password
You have not verified your account by clicking on the link we sent you via email. Please check your email folders (including your Spam folder) and click on the verify link sent.
Email is required
Password is required








Join FashionPotluck.com
Create your own profile in order to create content, follow other divas and like their posts, use our own messenger, and be a part of a growing international women community!
WELCOME TO OUR COMMUNITY
Fashion Potluck -
the first social media
platform for women.
You are free to read/watch & create content,
express your true self, and interact with others.
Join for free
Already a member? Log in here.
Purchase Alert
Dear Queen, you can only buy from one seller at the time. Please finish this purchase first in order to buy from another FP member
Comments
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
Please select one platform to continue
EDITOR APPROVED
You are wondering what is this 'Editor Approved'?
Well, this is pretty awesome! In order for the post to qualify and receive this accolade, it has to have a minimum of 700 words and two images (at least one original).
Receiving this accolade means two things: 1) Your content is amazing! Good job! 2) Your content qualifies for our monetization program. Every week two of the most read posts receive monetary rewards.
Have the badge & want to monetize your content?

LIFESTYLE
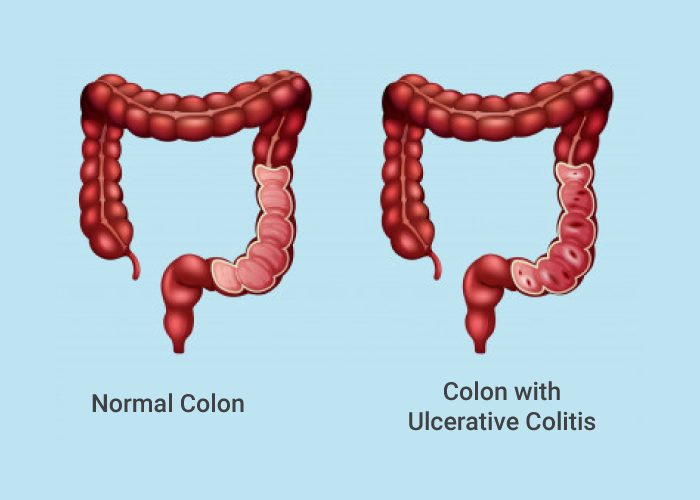
Ulcerative colitis is a long-term disease that can cause different symptoms in different people. Someone can have it without developing any symptoms, while others suffer from frequent flare-ups.
Regardless of the severity of the condition, it is still possible to effectively manage your abdominal pain and other symptoms, including diarrhea and weight loss. Taking medication, following a healthy diet, and reducing stress levels can all help decrease the chances of a flare.
To help your healthcare provider find out what is the culprit of your abdominal pain and other symptoms, you need to be able to accurately describe it. Try to keep a colitis symptom journal to write down what you are feeling.
You should also be reading to speak with a specialist about any negative emotions you might be experiencing. According to the U.S. National Library of Medicine, this is particularly true if you think you may suffer from depression, which can exacerbate existing pain.
Once you’ve described your pain in the right way, your doctor will likely be able to track down the root cause of your pain and begin treating it.
Let’s look at some ways to control chronic pain caused by ulcerative colitis. P.S. Some of these methods can also be helpful for people with chronic pain caused by any other conditions.
1. Reduce your stress levels
Stress is similar to depression, as it can worsen the pain and other symptoms of ulcerative colitis. Learning ways to manage stress through prescribed meditation, yoga, tai chi, or deep breathing might help reduce stress and, as a result, alleviate your pain from ulcerative colitis. If you can’t cope with stress on your own, talk to your physician or psychologist.
2. Talk to your doctor about surgery
Surgery is a long-lasting treatment approach for ulcerative colitis. The Crohn's & Colitis Foundation reports that 23 to 45 percent of people with ulcerative colitis might need surgery at some point, partially due to severe symptoms that no longer respond to medication.
Surgery options include a proctocolectomy (the removal of the rectum and all or part of the colon); a colectomy (the removal of all or part of the colon); and an ileostomy (a surgically created hole in the abdomen that allows waste to leave the body).
3. Adjust your diet
Though food doesn’t lead to ulcerative colitis itself, your diet has a huge impact on your symptoms. Diet can either trigger or ease them. You might find that eating a diet that’s low in certain sugars or fiber, especially insoluble fiber, which passes through the gastrointestinal tract undigested, or free of lactose or gluten helps you control your inflammatory bowel disease (IBD). Caffeine and carbonated drinks might also exacerbate your symptoms, as can spicy dishes. In some people, diet can provoke a flare.
4. Take medications according to your doctor’s prescription
It’s essential to stick to your prescribed medication regimen if you want to manage your pain and other symptoms effectively. There is a wide range of drugs your doctor can prescribe to treat your specific symptoms. Some of them can work by modifying your immune response which is crucial since ulcerative colitis is an autoimmune condition, while others are aimed at reducing the inflammation in your gut. If you skip doses or don’t take the medication as prescribed, you will reduce its effectiveness and run the risk of having a flare-up.
If you’re suffering from mild pain, a specialist might recommend acetaminophen, but you might have to avoid taking nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, since they can increase pain and exacerbate symptoms.
Comments
Related Posts
- Modern Female Leadership: Embracing the Technological Revolution by Sophia Smith 0
- Revitalize Without Surgery: Exploring Popular Non-Invasive Cosmetic Treatments by Erin Lane 0
- Understanding Lip Reduction Surgery: What You Need to Know by Monica Quinn 0
More Posts
- Travelling: Unlocking Singapore by Iuliana Roman-Popovici 0
- How to become a fashion stylist I Exclusive Course Discount by Una Omeragic 0
- Barcelona for Fashion Aficionados: The Essential Guide by Milly Grace 1
Vote content out
Reason for voting this content out?
Reason for voting this content out?

 Login with Google
Login with Google Login with Twitter
Login with Twitter






 by
by
Add Comments